Advertisment
ESOT 2013 Report – Today’s patients, tomorrow’s outcomes: how can we manage risk factors to improve graft survival in renal transplantation?

by Maria Dalby – Kidney transplants could in principle last forever – the common assumption that kidney transplants inevitably deteriorate and fail is not supported by the latest evidence.  This was the rationale for an Astellas sponsored satellite symposium at ESOT 2013 in which five distinguished speakers outlined how management protocols can be optimised to address all available risk factors and thus improve long-term outcomes.
This was the rationale for an Astellas sponsored satellite symposium at ESOT 2013 in which five distinguished speakers outlined how management protocols can be optimised to address all available risk factors and thus improve long-term outcomes.
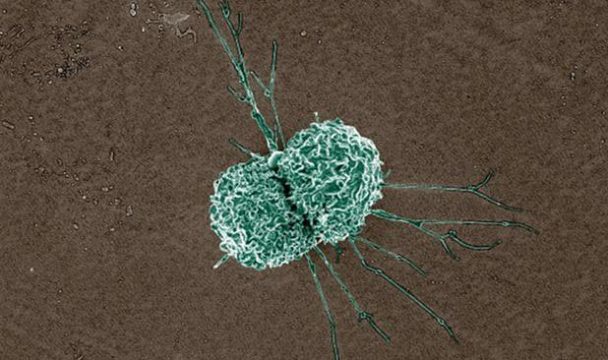
In the first session of the symposium, Dr Philip Halloran from University of Alberta set the scene by outlining the current status. Starting from the assumption that kidney graft failure always has an identifiable cause [3], Dr Halloran showed how the most common causes of graft loss can be prevented by optimising the immunosuppressive regimen. Graft dysfunction occurs when disease appears – most commonly antibody-mediated rejection (ABMR), followed by chronic glomerulonephropathy or polyomavirus infection [4]. Although immunosuppressive therapy has stabilised in the wake of the SYMPHONY study [5], data from a large multicentre study shows that centres often fail to diagnose ABMR correctly [6]. Dr Halloran stressed that there is a significant unmet need for improved tools for determining the molecular phenotype to inform therapeutic decisions, similar to the development seen in breast cancer [7]. Such tools will enable clinicians to detect signs of rejection and intervene at an early stage.
Factors that have been linked to graft loss include non-adherence to immunosuppressive therapy, variability in the exposure to immunosuppressive drugs, and exaggerated minimisation of immunosuppression to reduce the risk of nephrotoxicity. Dr Halloran agreed that it is reasonable to take steps to reduce the pharmacokinetic variability of immunosuppressive drugs – with any life-saving drugs – and ensure consistent exposure. However, he pointed out that the assumption that calcineurin inhibitor (CNI) immunosuppression causes progressive renal failure at therapeutic levels is no longer supported by the available evidence base and should not be part of the decision making process.
The topic of non-adherence to immunosuppressive therapy was discussed in detail by Professor Dirk Kuypers from Leuven in Belgium, who reminded the audience of the extensive body of evidence linking non-adherence to outcomes such as graft loss [8-11], graft dysfunction [12], late acute rejection [11-15], and chronic rejection [8, 16]. In addition, and importantly, more recent studies have documented a link between non-adherence and the development of de novo donor-specific human leukocyte antigen (HLA) antibodies (DSAs). In a prospective biopsy study of 315 renal transplant recipients, 60 patients developed graft failure – the majority of these failures (64%) were caused by ABMR, and in nearly half of these cases the investigator had noted non-adherence on the patient record [44]. A Canadian biopsy study showed that non-adherence was a significant independent predictor of the development of DSAs (OR 8.75, p<0.001) and that recipients who developed DSAs had significantly poorer 10-year graft survival than those who did not (57% vs 96%, p<0.0001) [2].
In the majority of cases, non-adherence is unintentional [17, 18]. Chronic medication and polypharmacy are known risk factors for non-adherence [19]. In addition, studies have shown that younger patients and/or patients with poor life satisfaction are more likely to be non-adherent [20]. Professor Kuypers was the principal investigator for the Adherence Measurement in Stable Renal Transplant Patients Following Conversion From Prograft to Advagraf (ADMIRAD) study which used electronic monitoring to evaluate whether switching from twice-daily to once-daily immunosuppressive treatment with tacrolimus could improve adherence in kidney transplant recipients [21]. A total of 219 patients were enrolled and received treatment with twice-daily tacrolimus before randomisation to either once-daily or twice daily tacrolimus for six months. Amongst the patients who remained on the therapy, a significantly higher proportion of patients in the once-daily group took the medication as prescribed (P=0.0009). Patients in the twice-daily group were significantly more likely to miss doses in the evening than in the morning, especially on Tuesdays and Saturdays, and the investigators concluded that eliminating the burden of the evening dose had the potential to improve adherence overall [21].
In the next session, Dr Klemens Budde from Berlin picked up the subject of variability in exposure to immunosuppressive therapy and how this may affect long-term outcomes. The CNI class is known for its narrow therapeutic index, which means clinicians must tread a precariously narrow path between under- and over-immunosuppression. Analysis of SYMPHONY data shows that tacrolimus trough levels were outside the target range in up to 50% of patients [22, 23]. Non-adherence is a major cause of intra-patient variability, but other factors may also play a role, including differences in gastrointestinal motility, diarrhoea, intake of food and/or other drugs, and variations in the timing of intake and/or testing [16, 24-29]. Several published studies have linked intra-patient variability in immunosuppressive exposure to graft failure [30-33], acute rejection [31-33], chronic rejection [34], impaired renal function [31, 32], and interstitial fibrosis and tubular atrophy [35].
Formulation of tacrolimus as a once-daily, prolonged-release preparation has eliminated asymmetric dosing of tacrolimus; not only does this improve non-adherence as shown by Professor Kuypers, but it also means the exact timing of the drug intake becomes less critical, and the impact of food intake and differences in motility will be less pronounced [36]. Switching from twice-daily to once-daily tacrolimus has been shown to significantly reduce the intra-patient coefficient of variation and the proportion of patients with high variability [37]. Dr Budde also stressed the importance of reducing variability when aiming for low tacrolimus trough levels; the lower the trough levels, the less room there will be for variation [38] and stabilising the trough levels is therefore essential for successful CNI minimisation.
The concept of CNI nephrotoxicity has its origins in the results of early experimental studies on cyclosporine which were applied to human biopsies for diagnostic purposes. Professor Daniel Serón of the Vall d’Hebron hospital in Barcelona devoted his session to explaining how more recent studies have revealed no specific histological signs of CNI nephrotoxicity at stable therapeutic doses, and that unrestricted minimisation and withdrawal may lead to serious complications. In terms of acute nephrotoxicity, tacrolimus has been shown to have a neutral haemodynamic effect in healthy subjects [39]. The picture is less clear in the case of chronic nephrotoxicity; a study involving more than 1,300 patients found that CNI toxicity accounted for only 0.7% of graft losses over 50 months [3]. CNI minimisation and withdrawal protocols have been shown to increase the rate of graft inflammation [40] and graft failure [41] and increase the risk of development of DSA and ABMR [1]. Patients who were maintained on stable trough levels of tacrolimus are significantly less likely to develop chronicity compared with patients with fluctuating levels [42]. Professor Serón concluded that whilst excessive trough levels of tacrolimus are associated with nephrotoxic risk, consistent exposure is the key to long term therapeutic success.
The importance of renal function and the clinical benefit of once-daily over twice-daily tacrolimus was also the topic of the concluding session of the symposium, presented by Dr Luis Guirado from Barcelona. Dr Guirado was one of the investigators on the EVOLUTION study which documented the efficacy, safety and patient preference for conversion from tacrolimus twice-daily to once-daily in more than 1,800 stable kidney transplant recipients in routine clinical practice [43]. The study showed that switching to an equivalent dose of once-daily tacrolimus maintained stable renal function and favourable tolerability with a very low (0.4%) rate of acute rejection. An overwhelming majority of patients (99.4%) expressed a preference for once-daily treatment, mainly because of losing the evening dose. Dr Guirado concluded that once-daily tacrolimus provides the means of maintaining the equilibrium between immunosuppression and nephrotoxicity that is essential for long-term graft survival.
References
1.Liefeldt, L., et al., Donor-specific HLA antibodies in a cohort comparing everolimus with cyclosporine after kidney transplantation. Am J Transplant, 2012. 12(5): p. 1192-8.
2.Wiebe, C., et al., Evolution and clinical pathologic correlations of de novo donor-specific HLA antibody post kidney transplant. Am J Transplant, 2012. 12(5): p. 1157-67.
3.El-Zoghby, Z.M., et al., Identifying specific causes of kidney allograft loss. Am J Transplant, 2009. 9(3): p. 527-35.
4.Halloran, P.F., et al., Antibody-mediated rejection, T cell-mediated rejection, and the injury-repair response: new insights from the Genome Canada studies of kidney transplant biopsies. Kidney Int, 2013.
5.Ekberg, H., et al., Reduced exposure to calcineurin inhibitors in renal transplantation. N Engl J Med, 2007. 357(25): p. 2562-75.
6.Halloran, P.F. and e. al., Microarray Diagnosis of antibody-Mediated Rejection in Kidney Transplant biopsies: an international prospective study (INTERCOM). Am J Transplant, 2013. in press.
7.Mirnezami, R., J. Nicholson, and A. Darzi, Preparing for precision medicine. N Engl J Med, 2012. 366(6): p. 489-91.
8.Didlake, R.H., et al., Patient noncompliance: a major cause of late graft failure in cyclosporine-treated renal transplants. Transplant Proc, 1988. 20(3 Suppl 3): p. 63-9.
9.Michelon, T.F., et al., Noncompliance as a cause of renal graft loss. Transplant Proc, 2002. 34(7): p. 2768-70.
10.Butler, J.A., et al., Frequency and impact of nonadherence to immunosuppressants after renal transplantation: a systematic review. Transplantation, 2004. 77(5): p. 769-76.
11.Denhaerynck, K., et al., Prevalence, consequences, and determinants of nonadherence in adult renal transplant patients: a literature review. Transpl Int, 2005. 18(10): p. 1121-33.
12.Vlaminck, H., et al., Prospective study on late consequences of subclinical non-compliance with immunosuppressive therapy in renal transplant patients. Am J Transplant, 2004. 4(9): p. 1509-13.
13.De Geest, S., et al., Incidence, determinants, and consequences of subclinical noncompliance with immunosuppressive therapy in renal transplant recipients. Transplantation, 1995. 59(3): p. 340-7.
14.Weng, F.L., et al., Race and electronically measured adherence to immunosuppressive medications after deceased donor renal transplantation. J Am Soc Nephrol, 2005. 16(6): p. 1839-48.
15.Nevins, T.E. and W. Thomas, Quantitative patterns of azathioprine adherence after renal transplantation. Transplantation, 2009. 87(5): p. 711-8.
16.Vasquez, E.M., et al., Medication noncompliance after kidney transplantation. Am J Health Syst Pharm, 2003. 60(3): p. 266-9.
17.Griva, K., et al., Non-adherence to immunosuppressive medications in kidney transplantation: intent vs. forgetfulness and clinical markers of medication intake. Ann Behav Med, 2012. 44(1): p. 85-93.
18.Gadkari, A.S. and C.A. McHorney, Unintentional non-adherence to chronic prescription medications: how unintentional is it really? BMC Health Serv Res, 2012. 12: p. 98.
19.Morales, J.M., E. Varo, and P. Lazaro, Immunosuppressant treatment adherence, barriers to adherence and quality of life in renal and liver transplant recipients in Spain. Clin Transplant, 2012. 26(2): p. 369-76.
20.Chisholm-Burns, M., et al., Factors related to immunosuppressant medication adherence in renal transplant recipients. Clin Transplant, 2012. 26(5): p. 706-13.
21.Kuypers, D.R., et al., Improved adherence to tacrolimus once-daily formulation in renal recipients: a randomized controlled trial using electronic monitoring. Transplantation, 2013. 95(2): p. 333-40.
22.Ekberg, H., et al., Cyclosporine, tacrolimus and sirolimus retain their distinct toxicity profiles despite low doses in the Symphony study. Nephrol Dial Transplant, 2010. 25(6): p. 2004-10.
23.Ekberg, H., et al., The challenge of achieving target drug concentrations in clinical trials: experience from the Symphony study. Transplantation, 2009. 87(9): p. 1360-6.
24.Venkataramanan, R., et al., Clinical pharmacokinetics of tacrolimus. Clin Pharmacokinet, 1995. 29(6): p. 404-30.
25.Schiff, J., E. Cole, and M. Cantarovich, Therapeutic monitoring of calcineurin inhibitors for the nephrologist. Clin J Am Soc Nephrol, 2007. 2(2): p. 374-84.
26.Antignac, M., et al., Population pharmacokinetics and bioavailability of tacrolimus in kidney transplant patients. Br J Clin Pharmacol, 2007. 64(6): p. 750-7.
27.de Jonge, H., M. Naesens, and D.R. Kuypers, New insights into the pharmacokinetics and pharmacodynamics of the calcineurin inhibitors and mycophenolic acid: possible consequences for therapeutic drug monitoring in solid organ transplantation. Ther Drug Monit, 2009. 31(4): p. 416-35.
28.Scholten, E.M., et al., AUC-guided dosing of tacrolimus prevents progressive systemic overexposure in renal transplant recipients. Kidney Int, 2005. 67(6): p. 2440-7.
29.Dew, M.A., et al., Rates and risk factors for nonadherence to the medical regimen after adult solid organ transplantation. Transplantation, 2007. 83(7): p. 858-73.
30.Borra, L.C., et al., High within-patient variability in the clearance of tacrolimus is a risk factor for poor long-term outcome after kidney transplantation. Nephrol Dial Transplant, 2010. 25(8): p. 2757-63.
31.Waiser, J., et al., Impact of the variability of cyclosporin A trough levels on long-term renal allograft function. Nephrol Dial Transplant, 2002. 17(7): p. 1310-7.
32.Clancy, M. and e. al., Presented at ESOT 2013.
33.Stevenson, K. and e. al., Presented at ESOT 2011., 2011.
34.Kahan, B.D., et al., Low intraindividual variability of cyclosporin A exposure reduces chronic rejection incidence and health care costs. J Am Soc Nephrol, 2000. 11(6): p. 1122-31.
35.Stoves, J. and C.G. Newstead, Variability of cyclosporine exposure and its relevance to chronic allograft nephropathy: a case-control study. Transplantation, 2002. 74(12): p. 1794-7.
36.Alloway, R., et al., Conversion of stable kidney transplant recipients from a twice daily Prograf-based regimen to a once daily modified release tacrolimus-based regimen. Transplant Proc, 2005. 37(2): p. 867-70.
37.Abu-Elmagd, K.M., et al., Five hundred intestinal and multivisceral transplantations at a single center: major advances with new challenges. Ann Surg, 2009. 250(4): p. 567-81.
38.Ekberg, H., et al., Calcineurin inhibitor minimization in the Symphony study: observational results 3 years after transplantation. Am J Transplant, 2009. 9(8): p. 1876-85.
39.Zaltzman, J.S., A comparison of short-term exposure of once-daily extended release tacrolimus and twice-daily cyclosporine on renal function in healthy volunteers. Transplantation, 2010. 90(11): p. 1185-91.
40.Seron, D., et al., Reliability of chronic allograft nephropathy diagnosis in sequential protocol biopsies. Kidney Int, 2002. 61(2): p. 727-33.
41.Opelz, G. and B. Dohler, Effect on kidney graft survival of reducing or discontinuing maintenance immunosuppression after the first year posttransplant. Transplantation, 2008. 86(3): p. 371-6.
42.Naesens, M., et al., Tacrolimus exposure and evolution of renal allograft histology in the first year after transplantation. Am J Transplant, 2007. 7(9): p. 2114-23.
43.Guirado, L., et al., Efficacy and safety of conversion from twice-daily to once-daily tacrolimus in a large cohort of stable kidney transplant recipients. Am J Transplant, 2011. 11(9): p. 1965-71.
44.Sellares, J., et al., Understanding the causes of kidney transplant failure: the dominant role of antibody-mediated rejection and nonadherence. Am J Transplant, 2012. 12(2): p. 388-99.