Advertisment
ASH 2014: T-cell lymphomas: a challenge for clinicians
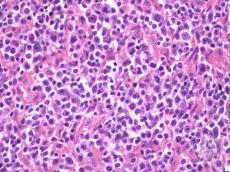
by Thomas R. Collins: Treating patients with T-cell lymphomas is fraught with challenges, requiring new approaches and sharper diagnosis, said Timothy Illidge, MD, PhD, Professor of Targeted Therapy and Oncology at the University of Manchester, who spoke here as part of a satellite symposium held before the 56th Annual Meeting of the American Society of Hematology.
Dr. Illidge gave an overview of T-cell lymphomas, which represent 10% to 15% of all non-Hodgkin lymphoma worldwide, and the difficulty clinicians have faced in trying to improve outcomes.These were among his points:
- Failure-free survival (FFS) rates are woefully low. Findings from the International T Cell Project (ITCP) — with 1,314 cases — show that 85% of patients received standard CHOP therapy (a combination of cyclophosphamide, doxorubicin, vincristine and prednisone). Even patients with the disease type that has the most favorable outlook, ALK-positive anaplastic large cell lymphoma (ALCL), achieved a failure-free survival rate of just 60%. (1) For ALK-negative ALCL patients, it was 36%. For angioimmunoblastic T cell lymphoma, it was 18%.
- Better diagnoses are needed in certain types. In the ITCP, which included some of the world’s foremost experts, a consensus of at least 3 of the 4 pathologists was reached only in 74% to 81% of ALK-negative ALCL, AITL, and PTCL not otherwise specified. “This is going to become increasingly important as we develop personalized therapies according to the biology and distinguishing the subtype of PTCL is going to become critical,” Dr. Illidge said. “So we need to get this right to begin to give the right treatments to the right patients.”
- Identifying risk factors for progression doesn’t do much to help tailor treatment. In the ITCP, the 5-year failure-free survival was 34% for angioimmunoblastic T-cell patients with zero and 1 risk factor from the International Prognostic Index. For those with PTCL not otherwise specified, it was 33%. So reducing therapy is not appropriate in those patients. A lower number of risk factors might play a role in ALK-positive ALCL, but it can only go so far. Those with one risk factor, or none, had an 80% FFS, and those with 2 had a 60% rate. But for those with 3, the rate dropped to 40%; and for those with 4 or 5 risk factors, it was 25%. Those over the age of 40 are at a particular risk of progression. “This really makes an important point: that ALK-positive patients with high IPI (risk factors) really are not doing well with CHOP alone,” he said. “And those patients over the age 40 — these patient should be treated as high-risk patients, similar to patients who present with less favorable T-cell lymphomas,” even though “this is a group of patients that traditionally have been thought to be doing really very well.” He summed up CHOP treatment this way: “Nobody likes it but most people still use it.”
Andrei Shustov, MD, Assistant Professor in the Hematology Division at the University of Washington School of Medicine, said that the understanding of the biology of these malignancies has grown tremendously in recent years, providing a good underpinning for developing better treatments. “In the last five to seven years we’ve really seen dramatic change in paradigm,” he said. “We understand these diseases.”
Steven Rosen, MD, Provost and Chief Scientific Officer at City of Hope in Duarte, Calif., turned to one of the biggest challenges in T-cell lymphoma treatment: those who relapse, a common occurrence with these diseases. Newer agents that have been studied show fairly good response rates in these patients, but the results often don’t last. The alkalylating agent bendamustine, for example, has produced an overall response rate of 50% in relapsed or refractory T-cell lymphomas, but the median duration of response was just 3.5 months. (2) The results from brentuximab vedotin have been more encouraging, with good response rates, and generally longer durations of response, particularly in anaplastic large cell lymphoma. The more reliable path to a cure, he said, is transplant, which, he noted, yields much better results during the first remission than if transplant is delayed until a second remission period.
There are other agents now in the early stages of investigation.Crizotinib, an ALK and ROS1-inhibitor, is being studied in ALCL and diffuse large B-cell lymphoma, so far with an overall response rates of between 60% and 91%. In Phase 2 data, mogamulizumab, an anti-CCR4 monoclonal antibody, has shown overall response rates of more than 30% in PTCL and cutaneous T-cell lymphoma.“Sequential single-agent therapies remain a consideration for most patients,” Dr. Rosen said. “And clinical trials are critical to advance novel agents and strategies to treat these diseases.”
(1) Vose, Armitage, Weisenburger, et al. International Peripheral T-Cell and Natural Killer/T-Cell Lymphoma Study: Pathology Findings and
Clinical Outcomes. J Clin Oncol 26:4124-4130.
(2) Damaj G, Gressin R, Bouabdallah, et al. Results from a prospective, open-label, phase II trial of bendamustine in refractory or relapsed T-cell lymphomas: the BENTLY trial. J Clin Oncol 2013 Jan 1;31(1):104-10.