Advertisment
EHA 2018: Molecular profiling in multiple myeloma

In addition to clinical segmentation of MM patients as young or elderly and fit or frail, genetic factors convey important prognostic information and should be taken into account in risk assessments and treatment decisions, in the same way as in other haematological malignancies such as AML. Professor Faith Davies from UAMS opened an educational session at EHA 2018 in Stockholm with an overview of the clinical impact of molecular subgroups, molecular risk and clonal heterogeneity in MM.
Translocations and hyperdiploidy are known to be important myeloma-initiating events that result in the upregulation of key oncogenes that in turn drive the expression of genes under the influence of immunoglobulin strong enhancers.1 Together with acquired secondary events including MYC and jumping translocations, copy number changes, epigenetic alterations and somatic mutations these initiating events promote disease progression.2-5 Recent data from the Myeloma Genome Project, a large-scale collaboration between academia, industry and patient advocacy organisations which comprises integrated genomics from more than 1,200 patients with newly diagnosed MM, shows that in addition to the common mutations of KRASand NRAS which are found in more than 20% of patients, and BRAF which is found in around 10%, there is a large number of driver gene mutations in MM.6 Some of these mutations, including IDH1 and IDH2 have not been shown before, and Professor Davies pointed out that although they were present in only a very small proportion of patients these mutations may prove very useful, as they are present in high clonal fractions which suggests they represent early events and thus may provide targets for intervention.6 Oncogenic dependencies were identified between the genetic abnormalities, including between t(4;14) and mutations in FGFR3, DIS3 and PRKD2, between t(11;14) and mutations in CCND1 and IRF4, and between hyperdiploidy and gain11q, mutations in FAM46C and MYCrearrangements. The Myeloma Genome investigators suggested that abnormalities that develop as MM progresses are to some extent predetermined by the initiating events, rather than as a result of random genetic hits.6 This non-random association between genetic abnormalities could potentially be exploited to target therapies for improved clinical outcomes. Examples of such targeted therapies include BCL-2 inhibitor venetoclax which has been shown to be particularly effective in patients with t(11;14) in terms of clinical response and time to progression;7MEK inhibitor trametinib which has been shown to benefit patients with NRAS or KRAS mutations;8 and use of BRAFinhibitor vemurafenib in patients with the BRAF V600E mutation.9
As clinical outcomes in MM have improved and a large proportion of patients are surviving with MM for 10 years or longer, assessing molecular risk in MM patients is becoming increasingly important – both for the sake of the patients, to be able to counsel patients with poor prognoses, and for selecting relevant endpoints and stratification strategies in clinical trials. Until now, the International Staging System (ISS)10 and more recently the revised ISS (R-ISS)11 have been used to identify high-risk MM patients. The ISS is largely based on clinical parameters (serum albumin and β2-microglobulin [β2M]) and although the R-ISS does take into account the high-risk chromosomal abnormalities del(17p), t(4;14) and t(14;16) it does not include data on 1q gain or TP53 mutations. One aim of the Myeloma Genome Project is to identify high-risk MM patients where targeted therapy can improve outcomes; by integrating DNA drivers and clinical data from 784 patients into a Cox model of ISS, age, PFS, OS and genomic data, the Myeloma Genome investigators have shown that the distribution of genomic myeloma markers is independent of ISS stage which indicates that combining genetic factors with clinical features will result in improved prognostic models.6 In this dataset, bi-allelic alteration of TP53 and 1q amplification were found in 3.7% and 6.1% of patients, respectively, and were both associated with very poor survival outcomes.6 Patients with either of these chromosomal abnormalities and ISS stage III were described as having ‘double-hit’ myeloma; these patients will have a dire prognosis and should be considered for novel treatments.6
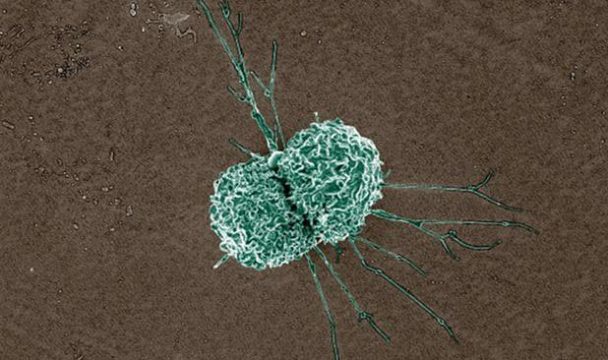
Myeloma cells are known to adapt to their microenvironment in a Darwinian fashion, ensuring survival of the fittest and progressing by repeated clonal sweeps which means different sites of disease can evolve differently.12-17 For this reason risk assessment should involve biopsies from multiple sites to identify any intra-patient heterogeneity, since a single high-risk sample out of discrepant samples is predictive of significantly poorer overall survival compared with two low-risk samples.18Targeting clonal heterogeneity at diagnosis to minimise its presence both over time and across sites will be key to improving long-term, outcomes in high-risk patients.
References
- Kuehl WM, Bergsagel PL. Multiple myeloma: evolving genetic events and host interactions. Nat Rev Cancer 2002;2:175-87.
- Walker BA, Leone PE, Chiecchio L, et al. A compendium of myeloma-associated chromosomal copy number abnormalities and their prognostic value. Blood 2010;116:e56-65.
- Walker BA, Wardell CP, Chiecchio L, et al. Aberrant global methylation patterns affect the molecular pathogenesis and prognosis of multiple myeloma. Blood 2011;117:553-62.
- Manier S, Salem KZ, Park J, et al. Genomic complexity of multiple myeloma and its clinical implications. Nat Rev Clin Oncol 2017;14:100-113.
- Pawlyn C, Kaiser MF, Heuck C, et al. The Spectrum and Clinical Impact of Epigenetic Modifier Mutations in Myeloma. Clinical Cancer Research 2016;22:5783-5794.
- Walker BA, Mavrommatis K, Wardell CP, et al. Identification of novel mutational drivers reveals oncogene dependencies in multiple myeloma. Blood 2018.
- Kumar S, Kaufman JL, Gasparetto C, et al. Efficacy of venetoclax as targeted therapy for relapsed/refractory t(11;14) multiple myeloma. Blood 2017;130:2401-2409.
- Heuck CJ, Jethava Y, Khan R, et al. Inhibiting MEK in MAPK pathway-activated myeloma. Leukemia 2016;30:976-80.
- Andrulis M, Lehners N, Capper D, et al. Targeting the BRAF V600E mutation in multiple myeloma. Cancer Discov 2013;3:862-9.
- Greipp PR, San Miguel J, Durie BG, et al. International staging system for multiple myeloma. J Clin Oncol 2005;23:3412-20.
- Palumbo A, Avet-Loiseau H, Oliva S, et al. Revised International Staging System for Multiple Myeloma: A Report From International Myeloma Working Group. J Clin Oncol 2015;33:2863-9.
- Greaves M, Maley CC. Clonal evolution in cancer. Nature 2012;481:306-13.
- Maley CC, Galipeau PC, Finley JC, et al. Genetic clonal diversity predicts progression to esophageal adenocarcinoma. Nat Genet 2006;38:468-73.
- Su F, Bradley WD, Wang Q, et al. Resistance to selective BRAF inhibition can be mediated by modest upstream pathway activation. Cancer Res 2012;72:969-78.
- Lee JC, Ahn KS, Jeong SJ, et al. Signal transducer and activator of transcription 3 pathway mediates genipin-induced apoptosis in U266 multiple myeloma cells. J Cell Biochem 2011;112:1552-62.
- Campbell PJ, Yachida S, Mudie LJ, et al. The patterns and dynamics of genomic instability in metastatic pancreatic cancer. Nature 2010;467:1109-13.
- Shah SP, Morin RD, Khattra J, et al. Mutational evolution in a lobular breast tumour profiled at single nucleotide resolution. Nature 2009;461:809-13.
- Rasche L, Chavan SS, Stephens OW, et al. Spatial genomic heterogeneity in multiple myeloma revealed by multi-region sequencing. Nat Commun 2017;8:268.